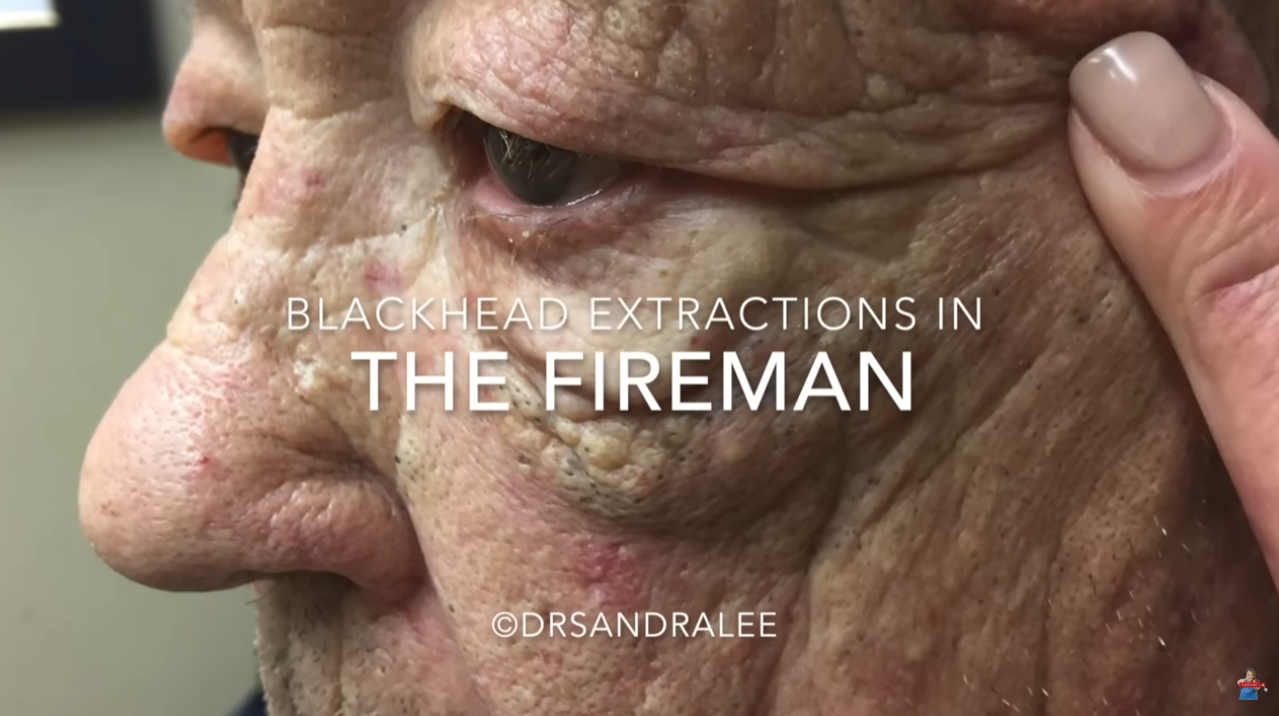
Extracting a giant blackhead (technically called a dilated comedo or, if very large and keratin-filled, a giant comedo or epidermal inclusion cyst with an open comedonal opening) in an 85-year-old requires special care due to age-related skin fragility, potential comorbidities, and slower healing.
⚠️ Important: This should only be performed by a qualified healthcare professional—ideally a dermatologist or trained clinician—not at home.
Here’s how it’s typically handled safely and ethically in a clinical setting:
🔍 1. Assessment First
- Rule out malignancy: In elderly patients, especially with longstanding or changing lesions, skin cancer (e.g., basal cell carcinoma, squamous cell carcinoma) can mimic a giant comedo.
- Evaluate for infection, inflammation, or underlying conditions (e.g., steatocystoma multiplex, favre–racouchot syndrome, or epidermal cysts).
- Review medications (e.g., anticoagulants) and comorbidities (e.g., diabetes, vascular disease) that affect healing or bleeding risk.
🧼 2. Sterile Preparation
- Cleanse the area with antiseptic (e.g., chlorhexidine or povidone-iodine).
- Use sterile gloves, instruments, and drapes — older skin is more prone to infection.
✂️ 3. Technique (varies by lesion type)
➤ For a true giant comedo (keratin plug):
- May use a sterile comedo extractor (loop tool) to gently apply pressure around the opening.
- Often, a small incision with a #11 blade is made to widen the follicular opening, allowing controlled expression.
- Keratinous material is expelled slowly — never force extraction, as this risks tearing the thin dermis.
➤ For a large epidermal cyst with a comedo-like opening:
- Requires a small incision (2–4 mm), then gentle expression + curettage of the sac.
- Some clinicians prefer minimal excision technique (MET), which preserves the sac for possible full removal later if recurrent.
🩹 4. Aftercare (Critical in elderly patients)
- Apply antibiotic ointment (e.g., mupirocin) if no allergy.
- Cover with a non-adherent sterile dressing.
- Monitor for signs of infection (redness, swelling, pus, fever).
- Avoid adhesive tape directly on fragile skin—use paper tape or silicone-based dressings.
❗ Special Considerations in 85-Year-Olds:
- Skin atrophy: Thinned epidermis and dermis → high risk of tearing.
- Poor wound healing: Nutritional status, circulation, and comorbidities matter.
- Pain sensitivity: Topical lidocaine (e.g., EMLA cream) or local infiltration may be needed.
- Patient comfort/mobility: Positioning must avoid strain or falls.
✅ When to Avoid Extraction:
- If the lesion is inflamed, infected (→ treat infection first).
- If bleeding risk is high (e.g., on anticoagulants without clearance).
- If patient is immunocompromised or has uncontrolled diabetes.
📌 Bottom line: Extraction is possible, but must prioritize safety over immediacy. Referral to dermatology is strongly advised for elderly patients with large or atypical facial lesions.
Let me know if you’d like visuals (e.g., diagrams of tools/techniques) or guidance on post-procedure wound care protocols for fragile skin.
🔬 Definition & Differential Diagnosis
A giant comedo (also called giant open comedo or giant keratin plug) is a markedly dilated pilosebaceous follicle filled with compacted keratin and sebum, with a visibly enlarged follicular opening and black-oxidized surface. While most common on the face (especially nose, cheeks), they may occur on the back or chest.
In elderly patients, key differentials include:
- Epidermal (infundibular) cyst with ruptured/opened wall
- Favre–Racouchot syndrome (nodular elastosis with cysts/comedones in sun-damaged skin)
- Trichilemmal cyst
- Keratinizing basal cell carcinoma or trichoblastoma
- Proliferating epidermoid cyst (rare, potentially malignant transformation)
- Sebaceous adenoma/carcinoma (especially in Muir-Torre syndrome)
📌 Critical: Any atypical, rapidly enlarging, bleeding, or ulcerated lesion in the elderly warrants biopsy before manipulation.
Reference: Bolognia JL, Schaffer JV, Cerroni L (eds.). Dermatology, 5th ed. Elsevier, 2023. Chap 82 (Cysts & Pseudocysts); Chap 110 (Neoplasms of the Pilosebaceous Unit).
🩺 Step-by-Step Clinical Protocol
1. Pre-Procedure Evaluation
2. Informed Consent & Risk Disclosure
In geriatric patients, emphasize:
- Risk of skin tearing (due to dermal atrophy, elastosis, or steroid use)
- Delayed healing (average epidermal turnover in >80 y/o is ~80 days vs. 28 days in young adults)
- Infection: S. aureus colonization prevalence >30% in elderly institutionalized patients
- Scarring or dyspigmentation
Document capacity assessment if cognitive impairment is suspected.
Ref: American Geriatrics Society. AGS Ethical Guidelines for the Delivery of Health Care to Older Adults. J Am Geriatr Soc. 2020;68(1):192–198.
3. Preparation & Anesthesia
4. Extraction Technique
🧰 Instruments:
- #11 scalpel blade
- Sterile comedo extractor (large loop, e.g., 6–8 mm diameter)
- Iris or fine forceps
- Curette (2–3 mm, blunt-tipped)
- Gauze or cotton-tipped applicators
📋 Procedure:
- Incision (if needed)
- For a true giant comedo with a tight orifice: make a tiny vertical nick (2–3 mm) over the center of the plug using #11 blade—do not cut deeply; aim for intrafollicular plane (epidermis only).
- For cystic lesions: small linear incision at the comedonal pore.
- Expression
- Place comedo extractor loop around (not on) the lesion.
- Apply gentle, sustained circumferential pressure—never focal squeezing.
- Keratin plug should extrude as a dense, cylindrical or conical cast (often segmented).
- Use cotton-tipped applicator to coax material out if adherent.
- Curettage (optional)
- If residual keratin remains, use blunt curette to gently scoop—avoid scraping dermis.
- Do not attempt full cyst wall removal unless excision planned (high rupture/inflammation risk in elderly).
- Hemostasis
- Light pressure with sterile gauze × 2–3 min.
- Avoid silver nitrate (causes tissue necrosis, delays healing in aged skin).
- For persistent oozing: aluminum chloride 20% solution or light electrocautery on low setting (≤1–2 W).
📌 Note: In Favre–Racouchot, multiple giant comedones are common; extract only symptomatic/bothersome ones—avoid aggressive clearing due to skin fragility.
Ref: Gupta G, et al. Surgical Pearl: The Mini-Incision Technique for Removal of Giant Comedones. Dermatol Surg. 2008;34(9):1265–1266.
Ref: Lee JB, et al. Favre-Racouchot Syndrome: Clinical and Histopathologic Study of 14 Cases. Am J Dermatopathol. 2011;33(3):225–229.
5. Post-Procedure Management
Ref: Koyano S, et al. Wound Healing in the Elderly: Current Therapies and Future Directions. Rejuvenation Res. 2021;24(5):407–415.
Ref: Levenson SM, et al. The Moist Wound Healing Principle: Scientific Evidence. J Wound Care. 1994;3(3):147–150.
⚠️ Contraindications to Extraction in Elderly
📚 Key Supporting References
- Bolognia JL, Schaffer JV, Cerroni L (eds.). Dermatology, 5th ed. Elsevier, 2023.
- Chapters 82 (Cysts), 110 (Pilosebaceous Neoplasms), 13 (Aging Skin)
- Zaenglein AL, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74(5):945–973.
→ Discusses comedo pathophysiology and extraction safety. - Gupta G, et al. Surgical Pearl: The Mini-Incision Technique for Removal of Giant Comedones. Dermatol Surg. 2008;34(9):1265–1266.
→ Describes low-trauma technique adaptable for elderly. - Koyano S, et al. Wound Healing in the Elderly: Current Therapies and Future Directions. Rejuvenation Res. 2021;24(5):407–415.
→ Evidence on delayed re-epithelialization, collagen deficits, and optimal dressings. - American Geriatrics Society Beers Criteria® Update Expert Panel. J Am Geriatr Soc. 2023;71(7):2052–2069.
→ Guidance on analgesic/antibiotic selection in >65 y/o.
🧴 I. Non-Surgical (Medical) Solutions & Treatments
✅ When Medical Therapy Is Preferred Over Extraction
- Multiple comedones (e.g., Favre–Racouchot syndrome)
- Frail skin, high bleeding/infection risk
- Patient/caregiver preference for conservative approach
- Lesions are asymptomatic or minimally bothersome
🔬 A. Topical Therapies (First-Line, Low-Risk)
📌 Geriatric Tip: Start with once-weekly application × 2 weeks, then titrate up. Monitor for:
- Excessive dryness → ↑ TEWL (transepidermal water loss)
- Contact dermatitis (↑ prevalence in aged skin)
- Adherence issues (use pump dispensers, not jars)
💊 B. Oral/Systemic Therapies (Reserved for Severe/Refractory Cases)
❗ Avoid:
- Oral tetracyclines (doxycycline > minocycline): ↑ vestibular toxicity (dizziness/falls) in elderly
- Oral contraceptives: thromboembolism risk
- High-dose isotretinoin: high risk of mucocutaneous toxicity, hyperlipidemia, depression
🧼 II. Adjunctive & Supportive Care
🌞 A. Photoprotection
- Daily broad-spectrum SPF 30+ (mineral: ZnO/TiO₂) — critical in Favre–Racouchot (UV is primary driver).
- Ref: Rigel DS, et al. Sunscreens: classification, photoprotection, and controversies. J Am Acad Dermatol. 2022;86(4):719–730.
- Use tinted formulations to improve adherence and provide visible light protection.
💧 B. Skin Barrier Support
- Moisturizers with ceramides, cholesterol, fatty acids (e.g., CeraVe®, EpiCeram®):
→ Restore stratum corneum integrity, ↓ irritation from actives
→ Apply within 3 min of bathing - Ref: Draelos ZD. The science behind skin care: moisturizers. J Cosmet Dermatol. 2018;17(2):138–144.
🧽 C. Gentle Cleansing
- Non-foaming, soap-free, pH 5.5 cleansers (e.g., Cetaphil Gentle Skin Cleanser, Vanicream Cleanser)
- Avoid washcloths/exfoliating scrubs (↑ microtears)
- Wash ≤1×/day in winter/dry climates
🛠 III. Procedure-Based Treatments (Beyond Extraction)
🚫 Avoid in elderly:
- Deep peels (phenol) → prolonged healing, cardiac risk
- Aggressive CO₂ laser → scarring, hypopigmentation
- Manual dermabrasion → bleeding, infection