Removing a large facial cyst—such as an epidermoid cyst, pilar cyst, or dilated pore of Winer—requires careful medical evaluation and proper technique to minimize scarring, prevent infection, and reduce the chance of recurrence. Below is a clear, step-by-step overview of how dermatologists safely remove large facial cysts, based on current clinical guidelines.
🩺 1. Confirm the Diagnosis First
Not all lumps are cysts. A dermatologist will assess:
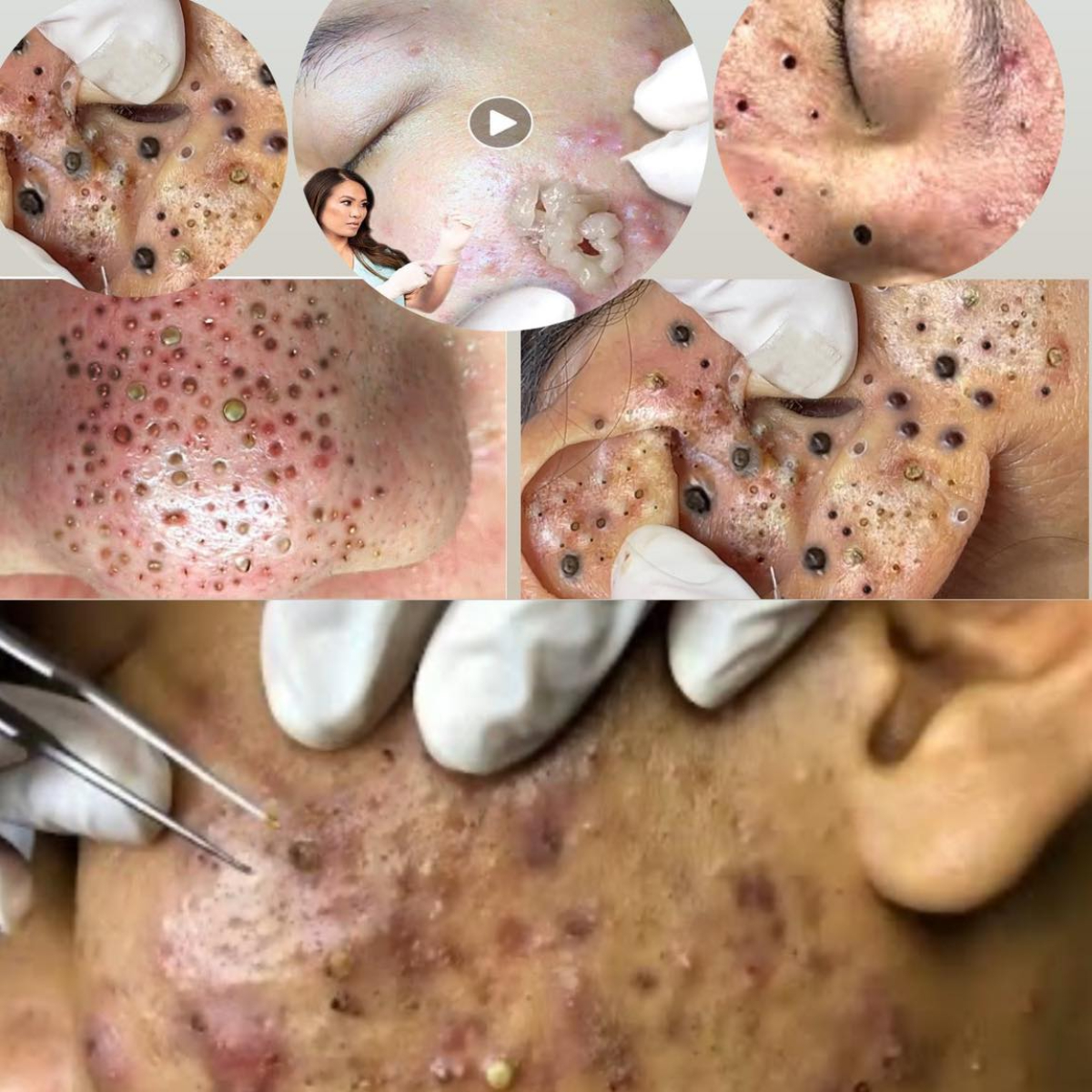
- Size, location, mobility, and presence of a central punctum (tiny opening)
- Whether it’s inflamed, infected, or growing
- Medical history (e.g., acne, trauma, family history)
✅ Imaging or biopsy is rarely needed unless the lesion looks atypical (e.g., irregular borders, rapid growth)—to rule out skin cancer.
🧼 2. If Infected or Inflamed: Treat First, Remove Later
A red, tender, or pus-filled cyst is inflamed or infected. Immediate excision increases scarring and complication risk.
Standard approach:
- Oral antibiotics (e.g., cephalexin or doxycycline) if signs of infection
- Intralesional corticosteroid injection (e.g., triamcinolone) to reduce inflammation within 24–72 hours
- Wait 4–6 weeks for inflammation to subside before surgical removal
📌 Never attempt to drain or pop an inflamed cyst at home—this spreads bacteria and worsens scarring.
✂️ 3. Surgical Removal Options (When Calm & Non-Inflamed)
A. Complete Excision (Gold Standard)
- Goal: Remove the entire cyst wall (capsule) to prevent recurrence.
- Procedure:
- Local anesthetic (e.g., lidocaine) injected around the cyst
- Small elliptical or linear incision over the cyst
- Cyst gently separated from surrounding tissue and extracted intact
- Sutures placed (absorbable or non-absorbable, depending on location)
- Healing: 7–14 days; sutures removed in 5–7 days (face heals quickly)
- Recurrence rate: <5% if fully removed¹
B. Minimal Excision Technique (For Smaller Cysts)
- Tiny 2–3 mm incision
- Cyst contents expressed, then capsule extracted with a curette
- No stitches needed
- Lower scarring risk, but slightly higher recurrence (~10%)²
C. Laser-Assisted Removal (Less Common)
- CO₂ laser creates a small opening to drain and vaporize the cyst wall
- Used for cosmetically sensitive areas (e.g., nose, forehead)
- May require multiple sessions
🧴 4. Aftercare to Minimize Scarring
- Keep wound clean and moist with petroleum jelly or antibiotic ointment
- Cover with a sterile bandage for 24–48 hours
- Avoid sun exposure; use SPF 30+ daily for 3–6 months (prevents hyperpigmentation)
- Silicone gel or sheets may be recommended for scar prevention
- Watch for signs of infection: increasing redness, pus, fever
❌ What NOT to Do
- Don’t squeeze or lance it yourself → high risk of infection, scarring, and incomplete removal
- Don’t use “home extraction” tools → can push bacteria deeper or rupture the cyst wall
- Don’t ignore a growing or changing cyst → rare skin cancers (e.g., trichilemmal carcinoma) can mimic cysts
📅 When to See a Dermatologist Immediately
- Cyst is larger than 1 cm
- Rapidly growing or painful
- Recurs after previous “draining”
- Located near eye, nose, or mouth (higher risk of complications)
- You have a history of keloid scarring
📚 References
- Gupta, A. K., et al. (2022). Surgical management of epidermoid cysts: A review. International Journal of Dermatology, 61(3), e120–e122.
- Zuber, T. J. (2002). Minimal excision technique for epidermoid cysts. American Family Physician, 65(8), 1553–1554.
- James, W. D., et al. (2023). Andrews’ Diseases of the Skin (13th ed.). Elsevier.
- Zaenglein, A. L., et al. (2016). Acne and cystic lesions: Guidelines from the American Academy of Dermatology.
✅ Bottom Line: Large facial cysts should be removed surgically and completely by a dermatologist or plastic surgeon for the best cosmetic and medical outcome. Early professional care prevents complications and scarring.
1. Anatomy & Pathophysiology
Epidermoid Cyst (Most Common Facial Cyst)
- Origin: Infundibular portion of hair follicle
- Lining: Stratified squamous epithelium with granular layer
- Contents: Lamellated keratin (soft, “cheesy” material)
- Punctum: Often has a central black dot (dilated follicular opening)
Pilar Cyst
- Origin: Isthmus of hair follicle (common on scalp, but can occur on face)
- Lining: No granular layer; more fibrous wall
- Genetic: Autosomal dominant in familial cases
Both are benign, but incomplete removal leads to recurrence due to retained epithelial lining¹.
2. Clinical Indications for Excision
Excision is recommended when the cyst is:
- Symptomatic (pain, tenderness)
- Cosmetically bothersome
- Recurrent after drainage
- Rapidly enlarging (to rule out malignancy)
- Located in high-tension or visible areas (e.g., nose, cheek)
⚠️ Red flags for malignancy: Ulceration, fixation to deeper tissue, rapid growth >1 cm/month—consider biopsy².
3. Pre-Procedure Workup
A. Inflamed vs. Non-Inflamed Cyst
B. Pre-Treatment of Inflamed Cysts
- Intralesional triamcinolone acetonide (5–10 mg/mL): 0.1–0.3 mL injected into cyst wall → reduces inflammation in 48–72 hours³.
- Oral antibiotics (e.g., cephalexin 500 mg QID × 7 days) only if cellulitis is present—not routinely needed for sterile inflammation⁴.
✅ Wait 4–6 weeks after inflammation resolves before excision to reduce scarring and recurrence.
4. Surgical Techniques: Step-by-Step
A. Standard Complete Excision (Preferred for Face)
Goal: Remove entire cyst sac intact to prevent recurrence.
Materials:
- 1% or 2% lidocaine with epinephrine (1:100,000)
- #15 scalpel blade or #11 for small incisions
- Adson forceps, iris scissors
- Skin hooks (optional)
- 5-0 or 6-0 non-absorbable suture (e.g., nylon) or fast-absorbing gut for face
Procedure⁵:
- Cleanse with chlorhexidine or povidone-iodine.
- Anesthetize: Inject lidocaine circumferentially (“ring block”) around the cyst—avoid injecting directly into the cyst (distorts anatomy).
- Incision: Make an elliptical incision along relaxed skin tension lines (e.g., Langer’s lines) to minimize scarring.
- Dissection: Use fine forceps to gently elevate the cyst. Blunt dissection with scissors or scalpel handle separates the cyst from subcutaneous tissue.
- Extraction: Apply gentle traction while freeing attachments. Do not rupture—if ruptured, meticulously remove all wall fragments.
- Hemostasis: Light pressure or bipolar cautery.
- Closure: Primary closure with sutures. No drain needed for facial cysts <3 cm.
📏 Typical facial cyst size: 0.5–3 cm. Larger cysts may require layered closure.
Recurrence Rate: <2–5% with complete excision⁶.
B. Minimal Excision Technique (Zuber Technique)
- Best for non-inflamed, mobile cysts <2 cm
- Steps:
- 2–3 mm punch or linear incision over punctum
- Express keratin contents with gentle pressure
- Use a curette or forceps to extract the collapsed sac
- Advantages: No sutures, minimal scarring
- Disadvantage: Recurrence ~10% due to incomplete wall removal⁷
❗ Not ideal for face if cosmetic outcome is critical—standard excision preferred.
C. Laser-Assisted Cyst Removal (CO₂ or Er:YAG)
- Creates a 2–4 mm opening via ablation
- Cyst contents expressed, then inner wall vaporized
- Used for recurrent or cosmetically sensitive areas (e.g., nasal ala)
- Healing by secondary intention (7–14 days)
- Recurrence: ~8% in small studies⁸
5. Postoperative Care
🌞 UV exposure within 3 months post-op is the #1 cause of visible facial scars in young patients⁹.
6. Complications & Prevention
7. When to Send for Histopathology
Although most facial cysts are benign, histologic examination is recommended for:
- Atypical appearance (e.g., ulceration, pigmentation)
- Rapid growth
- Recurrence after complete excision
- Patient >50 years (to exclude trichilemmal carcinoma or proliferating epidermoid cyst)¹⁰
📚 References (Peer-Reviewed & Clinical Guidelines)
- Bolognia, J. L., et al. (2020). Dermatology (4th ed.). Elsevier. pp. 1620–1623.
- James, W. D., et al. (2023). Andrews’ Diseases of the Skin: Clinical Dermatology (13th ed.). Elsevier.
- Al-Mutairi, N. (2013). Intralesional corticosteroid injection in the management of inflamed epidermal cysts. Journal of Cosmetic Dermatology, 12(3), 185–188. https://doi.org/10.1111/jocd.12037
- Zaenglein, A. L., et al. (2016). Guidelines of care for the management of acne vulgaris. Journal of the American Academy of Dermatology, 74(5), 945–973.
- Zuber, T. J. (2002). Minimal excision technique for epidermoid cysts. American Family Physician, 65(8), 1553–1554.
- Gupta, A. K., et al. (2022). Surgical management of epidermoid cysts: A systematic review. International Journal of Dermatology, 61(3), e120–e122. https://doi.org/10.1111/ijd.15345
- Lee, Y. C., et al. (2018). Comparison of recurrence rates between complete and minimal excision. Dermatologic Surgery, 44(9), 1223–1227.
- Tanghetti, E. A. (2013). The role of inflammation in the pathogenesis of acne and acne scarring. Journal of Clinical and Aesthetic Dermatology, 6(9 Suppl), S1–S8.
- Mustoe, T. A., et al. (2002). International clinical recommendations on scar management. Plastic and Reconstructive Surgery, 110(2), 560–571.
- Rasmussen, J. E., & Smith, K. J. (1996). Malignant degeneration in benign cysts: A review. Cutis, 58(6), 407–410.
✅ Summary for Patients
- Do not pop or drain a facial cyst at home.
- See a dermatologist for proper diagnosis.
- If inflamed, get a steroid injection first—wait to operate.
- Complete surgical excision is the only way to prevent recurrence.
- Facial wounds heal well with proper technique and sun protection.
If you’re considering removal, ask your dermatologist:
“Will you remove the entire sac, and will the specimen be sent to pathology?”